Mostrar el registro sencillo del ítem
dc.contributor.author
Perez Lloret, Santiago

dc.contributor.author
Negre Pages, Laurence

dc.contributor.author
Damier, Philippe

dc.contributor.author
Delval, Arnaud

dc.contributor.author
Derkinderen, Paul

dc.contributor.author
Destée, Alain

dc.contributor.author
Meissner, Wassilios G.

dc.contributor.author
Schelosky, Ludwig

dc.contributor.author
Tison, Francois

dc.contributor.author
Rascol, Olivier

dc.date.available
2017-05-08T22:09:09Z
dc.date.issued
2014-07
dc.identifier.citation
Perez Lloret, Santiago; Negre Pages, Laurence; Damier, Philippe; Delval, Arnaud; Derkinderen, Paul; et al.; Prevalence, determinants, and effect on quality of life of freezing of gait in Parkinson disease; Amer Medical Assoc; JAMA Neurology; 71; 7; 7-2014; 884-890
dc.identifier.issn
2168-6149
dc.identifier.uri
http://hdl.handle.net/11336/16126
dc.description.abstract
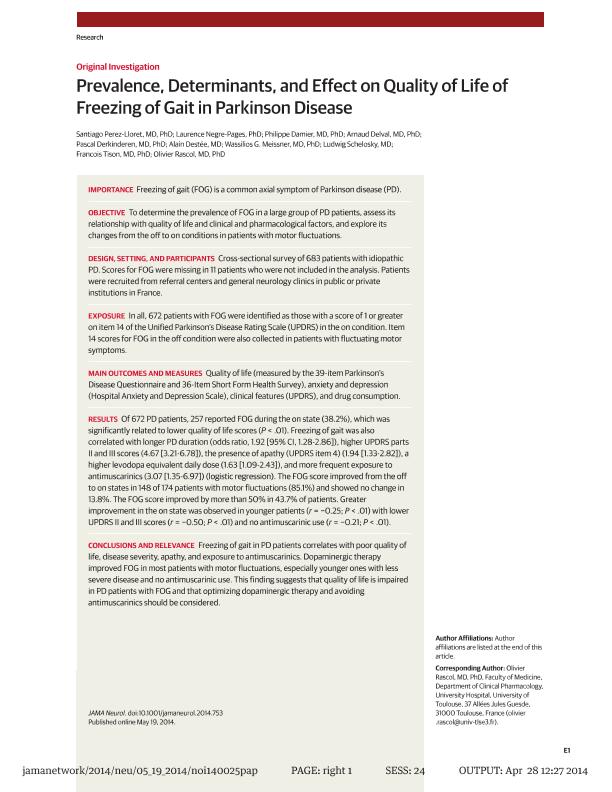
IMPORTANCE: Freezing of gait (FOG) is a common axial symptom of Parkinson disease (PD). OBJECTIVE: To determine the prevalence of FOG in a large group of PD patients, assess its relationship with quality of life and clinical and pharmacological factors, and explore its changes from the off to on conditions in patients with motor fluctuations. DESIGN, SETTING, AND PARTICIPANTS: Cross-sectional survey of 683 patients with idiopathic PD. Scores for FOG were missing in 11 patients who were not included in the analysis. Patients were recruited from referral centers and general neurology clinics in public or private institutions in France. EXPOSURE: Patients with FOG were identified as those with a score of 1 or greater on item 14 of the Unified Parkinson's Disease Rating Scale (UPDRS) in the on condition. Item 14 scores for FOG in the off condition were also collected in patients with fluctuating motor symptoms. MAIN OUTCOMES AND MEASURES: Quality of life (measured by the 39-item Parkinson's Disease Questionnaire and 36-Item Short Form Health Survey), anxiety and depression (Hospital Anxiety and Depression Scale), clinical features (UPDRS), and drug consumption. RESULTS: Of 672 PD patients, 257 reported FOG during the onstate (38.2%), which was significantly related to lower quality of life scores (P < .01). Freezing of gait was also correlated with longer PD duration (odds ratio, 1.92 [95% CI, 1.28-2.86]), higher UPDRS parts II and III scores (4.67 [3.21-6.78]), the presence of apathy (UPDRS item 4) (1.94 [1.33-2.82]), a higher levodopa equivalent daily dose (1.63 [1.09-2.43]), and more frequent exposure to antimuscarinics (3.07 [1.35-6.97]) (logistic regression). The FOG score improved from the off to on states in 148 of 174 patients with motor fluctuations (85.1%) and showed no change in 13.8%. The FOG score improved by more than 50% in 43.7% of patients. Greater improvement in the on state was observed in younger patients (r = -0.25; P < .01) with lower UPDRS II and III scores (r = -0.50; P < .01) and no antimuscarinic use (r = -0.21; P < .01). CONCLUSIONS AND RELEVANCE: Freezing of gait in PD patients correlates with poor quality of life, disease severity, apathy, and exposure to antimuscarinics. Dopaminergic therapy improved FOG in most patients with motor fluctuations, especially younger ones with less severe disease and no antimuscarinic use. This finding suggests that quality of life is impaired in PD patients with FOG and that optimizing dopaminergic therapy and avoiding antimuscarinics should be considered.
dc.format
application/pdf
dc.language.iso
eng
dc.publisher
Amer Medical Assoc

dc.rights
info:eu-repo/semantics/openAccess
dc.rights.uri
https://creativecommons.org/licenses/by-nc-sa/2.5/ar/
dc.subject
Parkinson Disease
dc.subject
Movement Disorders
dc.subject
Quality of Life
dc.subject
Medical Treatment
dc.subject.classification
Neurología Clínica

dc.subject.classification
Medicina Clínica

dc.subject.classification
CIENCIAS MÉDICAS Y DE LA SALUD

dc.title
Prevalence, determinants, and effect on quality of life of freezing of gait in Parkinson disease
dc.type
info:eu-repo/semantics/article
dc.type
info:ar-repo/semantics/artículo
dc.type
info:eu-repo/semantics/publishedVersion
dc.date.updated
2017-04-26T14:13:52Z
dc.identifier.eissn
2168-6157
dc.journal.volume
71
dc.journal.number
7
dc.journal.pagination
884-890
dc.journal.pais
Estados Unidos

dc.journal.ciudad
Chicago
dc.description.fil
Fil: Perez Lloret, Santiago. Universidad de Buenos Aires. Facultad de Farmacia y Bioquímica. Departamento de Farmacología; Argentina. University of Toulouse; Argentina. Inserm; Francia
dc.description.fil
Fil: Negre Pages, Laurence. LN Pharma; Francia
dc.description.fil
Fil: Damier, Philippe. Inserm; Francia. Centre Hospitalier Universitaire (CHU) Nantes; Francia
dc.description.fil
Fil: Delval, Arnaud. Centre Hospitalier Universitaire (CHU) Lille; Francia
dc.description.fil
Fil: Derkinderen, Paul. Inserm; Francia. Centre Hospitalier Universitaire (CHU) Nantes; Francia
dc.description.fil
Fil: Destée, Alain. Inserm; Francia. Centre Hospitalier Universitaire (CHU) Lille; Francia
dc.description.fil
Fil: Meissner, Wassilios G.. Centre National de la Recherche Scientifique; Francia. Centre Hospitalier Universitaire (CHU) Bordeaux; Francia. Universite de Bordeaux; Francia
dc.description.fil
Fil: Schelosky, Ludwig. Kantonsspital Münsterlingen; Suiza
dc.description.fil
Fil: Tison, Francois. Universite de Bordeaux; Francia. Centre National de la Recherche Scientifique; Francia. Centre Hospitalier Universitaire (CHU) Bordeaux; Francia
dc.description.fil
Fil: Rascol, Olivier. Inserm; Francia
dc.journal.title
JAMA Neurology
dc.relation.alternativeid
info:eu-repo/semantics/altIdentifier/doi/http://dx.doi.org/10.1001/jamaneurol.2014.753
dc.relation.alternativeid
info:eu-repo/semantics/altIdentifier/url/http://jamanetwork.com/journals/jamaneurology/fullarticle/1871698
Archivos asociados